RCM Solutions for Dental Practices and DSOs
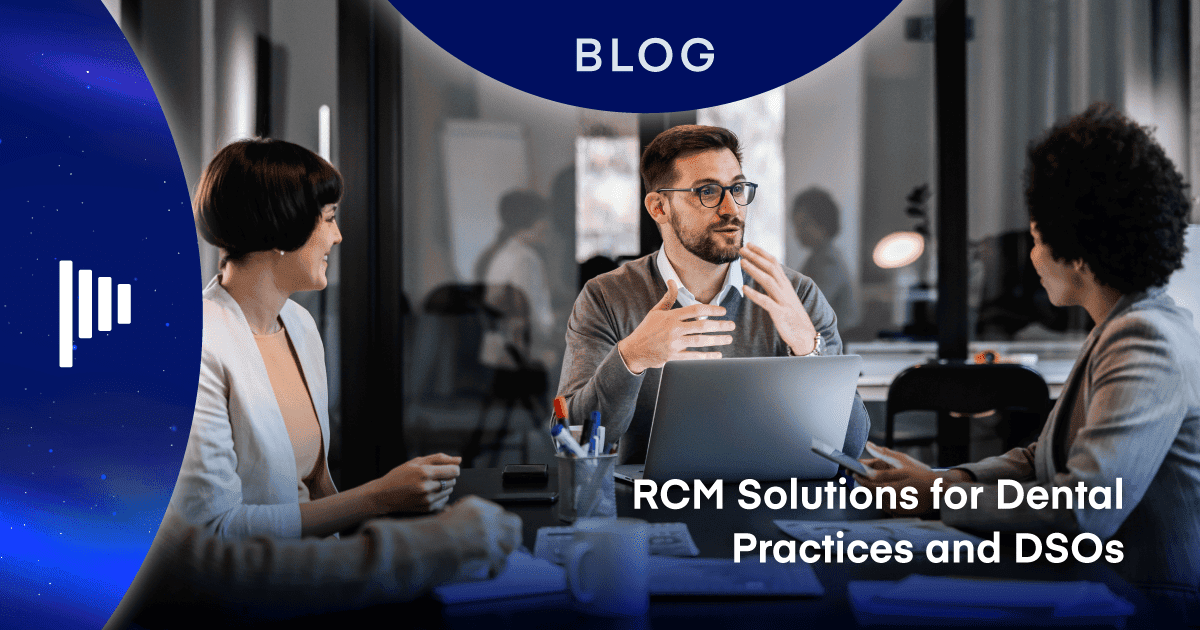
Revenue cycle management (RCM) is essential to the success of any dental practice. It’s all about ensuring that your dental services translate into actual revenue. However, managing RCM has traditionally been a labor-intensive process, prone to human error at every stage. With teams often working remotely, the need for easy and secure access to patient data is more crucial than ever.
Fortunately, cloud-based practice management systems are stepping in to streamline these processes, incorporating automation, workflow tools, reporting, and analytics to help dental service organizations (DSOs) optimize their RCM processes and boost practice management.
Read more about the challenges in our e-book: Solving the RCM Challenge for Dental Practices & DSOs
Automating RCM and Integrating Workflow Tools
Automation and integrated workflow tools are becoming essential for dental practices aiming to improve efficiency and enhance the patient experience.
As Jeremy Serfling, a revenue strategy expert at Planet DDS, puts it, “Top RCM priorities of private practices and DSOs include automation, greater access to insurance information, and integrated workflow tools. These are key to solving efficiency challenges and driving a positive patient experience.”
In response to these priorities, DSOs and dental groups have increasingly partnered with innovative solutions like Denticon and DentalXChange. These partnerships aim to streamline eligibility verification, expedite claims processing, and reduce the likelihood of errors—an effort that’s become even more critical as practices face staffing shortages and increased turnover.
Innovative Ways Denticon Improves RCM
Denticon integrated workflow with DentalXChange is a game-changer for dental practices. By reducing the time spent on manual processes, this integration allows team members to focus more on patient care. Additionally, because Denticon is cloud-based, team members with permission-based access can securely view data from remote locations, adding flexibility to operations.
Top Features of Denticon RCM
Denticon RCM comes with a range of key functionalities, including:
- Claims task manager: This tool replaces outdated methods like spreadsheets by managing outstanding claims directly within the system, ensuring nothing slips through the cracks.
- 835/ERA auto-posting payments: This feature automates the posting of payments to the ledger, significantly reducing the time spent on manual data entry and minimizing errors.
- RCM reporting: Denticon RCM reporting provides actionable insights that can be tailored by group or office, making it especially valuable for multilocation practices looking to quickly identify and address issues.
- Text and email payment reminders: Practices can send automated reminders to patients, offering them a convenient way to settle their accounts online.
- Card-on-file capability: This feature securely stores patients’ payment information, making the payment process more seamless and efficient.
These features not only streamline the RCM process but also ensure that dental practices are equipped to handle the complexities of modern-day billing and collections.
Payer Relations and Practice Operations
RCM encompasses two main components: payer relations and practice operations. Understanding these components is key to mastering the RCM process.
Victoria Johnson, founder of Top Tier Practice Solutions, emphasizes the complexities of dental insurance: “One of the reasons why dental insurance is so confusing is because it’s not insurance in the traditional sense. It’s a benefit plan determined by the employer.”
The negotiation of fees with insurance carriers, represented systematically through fee schedules, is a critical aspect of RCM. For DSOs, this can mean managing hundreds or even thousands of fee schedules within their practice management system. The intricacies of these negotiations directly impact the revenue cycle.
“When the practice receives back the explanation of benefits [EOB], it shows what you billed the insurance company according to your UCR [usual, customary, and reasonable charges], what the insurance carrier paid, which is the negotiated fee, and what is the difference between them,” explained Johnson.
“If the patient is correctly assigned to the correct fee schedule in your practice management system, then you receive from the insurance company what you expected to receive, and your ledger will balance out,” added Johnson.
Best Practices for RCM Operations
Whether it’s eligibility verification or claim submission, each step in the RCM process must be handled with precision. There are six core processes involved: eligibility verification, claim submission, claim follow-up, payment posting, denial management, and patient payment collection.
How to create successful RCM processes
Even with the best intentions, manual processes can lead to costly mistakes. Errors in patient scheduling, registration, and insurance verification are common, as are coding mistakes and delays in claim submissions. To mitigate these risks:
- Accuracy in patient information: Ensure that all patient information, from subscriber ID numbers to dates of birth, is entered correctly. Even minor mistakes can prevent claims from being processed.
- Automate insurance verification: Automating this process can save significant time and reduce the likelihood of errors. However, it’s important to understand the limitations of automation, as insurance carriers’ systems are often not well-organized.
- Timely claim submissions: Submitting claims on the same day as the service is crucial for ensuring timely payments. Delays can result in cash flow issues for the practice.
- Follow up on denials: Proactively managing denied claims is essential. Using tools like Denticon’s task manager can help prioritize and resolve outstanding claims efficiently.
Effective RCM Management for DSOs
Implementing a comprehensive and transparent RCM system is not just about technology—it’s about creating a culture of accountability and precision within your team. Regular training and well-defined standard operating procedures are crucial.
Cross-training team members ensures that the RCM process continues smoothly even if key personnel are unavailable. Additionally, standardizing the end-of-day process can help catch and correct errors before they become larger issues.
“It’s crazy how much money you can find in some practices,” said Victoria Johnson. “I know of one time when an office manager went out on vacation, and nobody went to the bank until she came back. Checks totaling tens of thousands of dollars were just sitting there in a drawer, instead of being deposited in the bank.”
Consistency is key when it comes to RCM, and having a reliable end-of-day checklist can make all the difference. Make sure to balance production, post checks, send claims, and balance collections daily. Performing end-of-day tasks in your practice management system ensures that everything matches up and reduces the risk of errors going unnoticed.
Discover Denticon to Improve RCM
Proper RCM processes, combined with the right practice management software, can transform your dental group’s financial health. By following best practices and leveraging automation, your practice can increase collections and profitability while delivering enhanced patient care.
Ready to take your RCM to the next level? Chat with our team about how Denticon can help your practice save time, increase revenue, and provide a better patient experience.